Pandemic in Africa: Lessons and Strategies
by Ramesh Thakur at Brownstone Institute
The following is an excerpt from Dr. Ramesh Thakur’s book, Our Enemy, the Government: How Covid Enabled the Expansion and Abuse of State Power.
Africa and the pandemic panic: Facts not fear
Africa is at risk of getting the worst of both worlds: failure to check the epidemic and failure to check economic collapse. Why?
First, because of a lack of state capacity, most African countries lack the administrations and health systems to implement and enforce “test, isolate, treat, and trace” regimes. What exactly does social distancing mean if you live in sprawling informal settlements that characterise almost all major cities in the developing world. Second, the dominance of the informal sectors and extreme dependence on daily wages to keep families afloat mean that economic disasters will deepen the misery of millions and multiply illnesses and deaths.
SARS-CoV-2 emerged through a chain not yet fully grasped in Wuhan, China and hitched a ride on the world’s flyways to insinuate itself into the very interstices of globalisation and spread rapidly to Iran, Europe, and North America. As at 15 May, the total number of Covid-19 (the disease caused by the virus) cases was 4.5 million and over 300,000 people had died with it worldwide. By any criterion, that is a serious pandemic.
But in perspective, the annual global deaths from leading causes is: coronary diseases 8.7 million, stroke 6.2 million, lung cancers and diseases 4.8 million, influenza and pneumonia 3.2 million, diabetes 1.6 million, and diarrhoea and tuberculosis 1.4 million each. So coronavirus does not represent the end of the world. People suffer but endure. This virus too shall pass and indeed is on the way down almost everywhere.
As of 13 May, the total number killed with Covid-19 in the 55 countries that make up the African Union was 2,382, or an average of 43 and a median of just 10 deaths per country. Algeria and Egypt are the only countries to record over 500 deaths. If we exclude them, the average falls to 1.3 deaths/week per country. That should not be enough to make it even to the inside pages of most newspapers, let alone disrupt life as we know it through massive shutdowns.
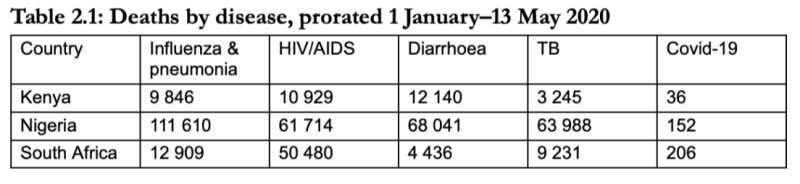
In comparison, Table 2.1 shows the top three killers in South Africa are HIV/AIDS (138,000 per year), heart diseases (41,000), and influenza and pneumonia (35,000); in Kenya they are diarrhoea (33,000), HIV/AIDS (30,000) and influenza and pneumonia (27,000); and in Nigeria they are influenza and pneumonia 305,460; diarrhoea 186,218, and tuberculosis 175,124.
What lessons can Africa learn from the experience of others thus far?
On 14 May, Mike Ryan, emergencies expert at the World Health Organisation (WHO), told an online briefing that the novel coronavirus “may become just another endemic virus in our communities, and this virus may never go away.” The statement from the WHO and the empirical reality of a very minor episode of the pandemic across Africa so far set the parameters of how Africa could address this particular “crisis:” as potentially but not presently a serious human security threat.
Africa has the opportunity to lead the world in an evidence-based rather than fear-driven approach and be an oasis of sanity and calm in a world gone collectively mad.
On 16 March, Imperial College London (ICL) published a fateful paper warning of up to 510,000 Covid-19 deaths in the UK and 2.2 million in the US without government intervention, and perhaps half those numbers without hard lockdowns of national economy and society. The model has been widely criticised by software engineers for its code and by medical scientists for its flawed assumptions and distorted data. Spooked by the crisis as it unfolded in real time in Italy and elsewhere and impressed as much by China’s accomplishment in suppressing it as by the grim curves of the ICL model, European, North American, Australasian and other governments imposed stringent lockdowns and social distancing requirements, often accompanied by instant heavy fines. The dominant media commentators, abandoning critical distance and objectivity, joined the herd to become pandemic panic addicts.
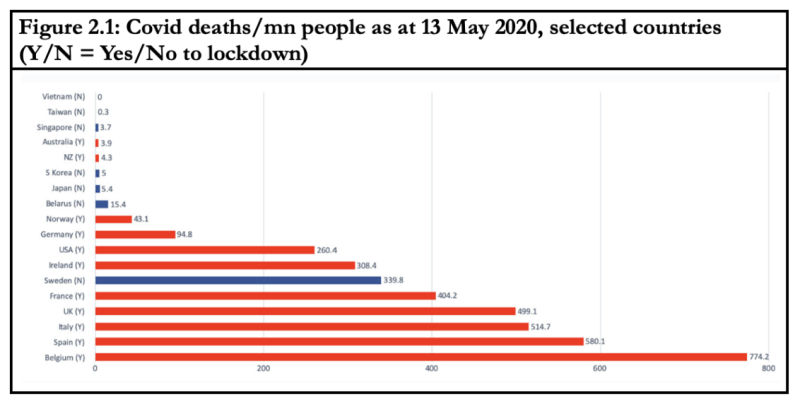
Figure 2.1 depicts the lack of correlation between lockdown measures and coronavirus deaths in selected countries. Restricting stringent lockdown measures to the elderly would have achieved most of the gains.
Applied to Sweden, Figure 2.1 is visually stunning in dramatising the discrepancy between two epidemiological models on either side and the empirical reality in the centre chart. Michael Levitt, a Chemistry Nobel Laureate, is on the mark with his caustic comment: “It seems that being a factor of 1,000 too high is perfectly OK in epidemiology.”
A three-pronged strategy for Africa: watch, prepare, and activate
Europe and North America combined, with just 14% of the world’s population, make up 75% and 86% of the world’s total of the coronavirus infected and dead. Asia, with 60% of the world’s population, accounts for only 16% and 8% of infections and dead. Astonishingly, Africa’s shares are 17%, 1.5% and 0.8%, respectively. The science behind the pandemic is poorly understood and no one has a satisfactory explanation for Africa’s great escape to date. That however is the factual reality. Accordingly, for now there is no need for African countries to take any immediate action for there is no crisis.
However, because the virus could evolve and strike suddenly and seriously, Africa should build up surveillance and testing capabilities across the continent, including at airports and seaports. Vigilance is the indispensable counterpart to caution sans panic.
It would also be prudent to undertake serological testing of population-representative samples to estimate the prevalence of antibodies and thus the spread of the infection. A second act of prudence would be to build the capacity to surge past the bottlenecks in the health and hospital systems, just in case a virulent mutation does strike suddenly.
The pandemic and the resulting socio-economic crises also highlight the need for global circuit-breakers to identify, isolate and quarantine systemic risks early. The crisis is an opportunity to reboot the ethic of global cooperation.
The WHO, which eradicated the scourge of smallpox in the 1970s, has a role in partnership with the African Union’s African Center for Disease Control (African CDC) in developing state capacity in African countries to manage epidemics that is essential and non-substitutable. This is why African countries should unite in resisting US efforts to belittle and destroy the WHO. Instead, they should seek the WHO and African CDC assistance to establish testing facilities and protocols; stockpile essential testing and protective equipment and therapeutic medicines; and build ICU capacity to cope with sudden surges of infections so “R”—the effective rate of virus reproduction—is kept below 1 all the time to ensure the threat recedes and does not proliferate.
Taking into account the low infection rates, living conditions, and economic realities, the test, isolate, treat, and trace approach seems to be a more appropriate policy response for Africa than panic-driven lockdown strategies whose consequences could kill more people than Covid-19 itself.
Pandemic in Africa: Lessons and Strategies
by Ramesh Thakur at Brownstone Institute – Daily Economics, Policy, Public Health, Society
Disclaimer
Some of the posts we share are controversial and we do not necessarily agree with them in the whole extend. Sometimes we agree with the content or part of it but we do not agree with the narration or language. Nevertheless we find them somehow interesting, valuable and/or informative or we share them, because we strongly believe in freedom of speech, free press and journalism. We strongly encourage you to have a critical approach to all the content, do your own research and analysis to build your own opinion.
We would be glad to have your feedback.
Source: Brownstone Institute Read the original article here: https://brownstone.org/

