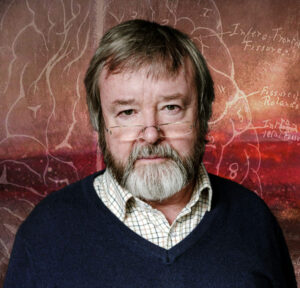
Is there a clinical case for psychedelic drugs? Professor David Nutt, a neuropsychopharmacologist, has spent his career trying to demonstrate that there is — and that, beyond their recreational powers, drugs such as psilocybin can effectively treat depression. Some of his advocacy has landed him in controversy: in 2009, he was dismissed from a governmental advisory position for his arguments about drug harms. But over the last decade, as more pharmaceutical companies and even the NHS look to psychedelic treatments, he appears to have been vindicated.
This week, Prof Nutt visited the UnHerd Club to discuss his latest research, the resistance he’s faced from the academic community and the transformative power of psychedelics. Below is an edited transcript of his conversation with Flo Read:
Florence Read: Instead of turning on parts of the brain, psychedelics can do something quite unusual, which is actually turn some parts off. Could you just explain a little bit more about that?
David Nutt: Obviously, Timothy Leary was wrong, these drugs don’t turn on the brain, they actually turn off the brain. Imaging work has shown that there’s a circuit in the brain called the “default mode network”, which controls how you think. Our research showed that network was being switched off.
You’ve probably heard of Aldous Huxley’s book The Doors of Perception. That book was written after a mescaline trip, but the phrase “the doors of perception” is taken from William Blake. And Blake said that: “If the doors of perception were cleansed every thing would appear to man as it is, Infinite. For man has closed himself up, till he sees all things thro’ narrow chinks of his cavern.” He was referring to people who aren’t artists, who see things in a very restricted way. Huxley used that quote, but he realised that what mescaline had done was open his mind, and then worked out that something must be closing his mind. What’s closing his mind? He said: the brain.
The brain is an instrument for focusing the mind. Psychedelics switch off the parts of the brain that control your mind. There was a group at Yale doing work in depression. They showed that the default mode network — the part of the brain that was turned off by psychedelics — is overactive in depression. If you scan the brains of depressed people, a greater amount of their brain is engaged in this internal, reflective, self-referential thinking. We thought: “Let’s see if we can turn it off in depressed people, and will they be non-depressed?” And lo and behold, they were.
We gave a single dose of psilocybin to people who had failed on other treatments. (They’d all failed on two antidepressants — somebody had failed on more than 10; they’d all failed on CBT.) They all got better. It’s the strongest effective treatment for resistant depression there’s ever been. Some of them are still well now, 10 years later. For the majority, the depression has crept back, and that tells us something else about the nature of how deeply embedded depressive thinking can be. But the fact that you could switch off the depression circuit, and lift people’s mood — that was a discovery.
FR: Among that cohort of treatment-resistant depressives, was there a common thread between them, in terms of their experience on the psilocybin? Or is it quite individualised?
DN: The content of a psychedelic trip is completely unpredictable. After that first trial, we set up a second trial, where we wanted to see if we could prolong the antidepressant effect of psilocybin by giving two trips, three weeks apart. And there was absolutely no relationship between the first trip and the second trip. Some people had a terrifying trip the first time, then a good one, and vice-versa.
What we try to do in therapy is get people to use the experience to deal with the thinking that is underpinning their depression. We asked them to try to engage with problems, to go back to issues in their childhood that might be relevant to their depression. Most of them don’t want to do that. One of the theories of depression — one of the theories about why your mind is so preoccupied in depression — is that you’re trying to resist re-engaging with those traumas. But we encouraged them to do that. It’s challenging, it’s difficult, they find it distressing — but they often get fundamental insights.
One of our patients on the first trial said: “I saw my father abusing me and I realised that was why I was depressed.” He realised: “I was blaming myself for the abuse. And in the trip, I was able to say to him, ‘That’s it.’” He got closure. He came out of the trip and he’s been well ever since. So people’s trips often focus on an individual trauma in their lives which they struggled to deal with. They have that in common.
FR: So given this level of success, why are these drugs not available for depressives in the UK?
DN: There are so many hurdles. Where to begin? The first is really weird. That initial study that we did was actually funded by the Medical Research Council. They put out a call for new treatments for depression and we got the grant. Getting the grant was the easiest bit. It took three iterations of the Ethics Committee to get permission to do this study. The ethics committee said: “It’s too dangerous; you can’t give depressed people psychedelics.” Why not? “Well, they might die.” That’s pretty unlikely — no one’s ever died on psilocybin before — but why do you think depressed people might die? “Well, they’re depressed.”
The third time we were going to this committee, I realised if we didn’t agree to do what they said, we would never get the study done. So in the end, they said: “You cannot do a controlled trial; you can do a safety study. Give 12 people it, see how they go. If none of them are dead in six months then you can come back and do a controlled trial.” So we said yes — in fact, the original trial was to see if people survived, which they all did. And the secondary outcome was whether their mood had changed. They could have got worse. They all got better.
So it took us a year to pass ethics. It took us another year to get hold of the medicine — the drug — because there’s only one place in the world that could make it. Then we had to get import licences and export licences. It took 30 months to get hold of the drug, and two more months to get permission from the Home Office to actually use it. That’s 32 months out of a 36-month grant — all because these drugs have been vilified for the last 50 years. The bureaucracy is so intense.
FR: Is this a bureaucracy problem or is it a moral failing?
DN: It’s more than moral; it’s political. The reason psychedelics were banned in 1967 in the US and in 1970 in the UK was simply because psychedelics were allowing people to think differently about how they wanted to run international relations. The war in Vietnam was being protested. There’s this amazing photograph I have, of someone holding a placard that says: “Drop acid, not bombs.” They couldn’t ban the anti-war protests so they banned the drugs instead, thinking that would dissipate the protests. Of course it didn’t, and eventually, the protesters won.
The Vietnam War ended but by that time, the drugs had been banned. And one of the worst things about drug laws is that it’s almost impossible to remedy them. For example, in America, two-thirds of states have medicalised cannabis, and half of states have recreational cannabis, but it’s still illegal under the federal law. In fact, there’s only two countries in the world that have actually pulled cannabis out of the UN conventions, and that’s Canada and Uruguay. Every other country in the world, even America, still complies with the UN regulations, which still say that cannabis is an illegal drug. And no country has pulled psychedelics out of the UN conventions.
So everything we do, we do in the face of this enormous barrier. They’ve created this myth that these are very dangerous. Almost everything you’ve heard about psychedelics has actually been a deliberate misrepresentation to perpetuate this political decision that people shouldn’t use them.
FR: Would the power dynamic between a doctor and a patient change if this kind of drug became legalised?
DN: The medical profession isn’t really that progressive. And I can say that: I’m a doctor. I have become more and more disappointed by the inability of medicine — particularly in fields like psychiatry — to move with the times. I personally think that psychedelics will re-energise psychiatry. A lot of psychiatrists are very disillusioned. We haven’t had any real innovation in psychiatric medicine or psychiatric psychotherapy for 50 years.
FR: One thing under threat at the moment is the idea of holistic health — the idea that your mind and body have some sort of co-dependent relationship.
DN: We are quite top-down, paternalistic and autocratic in healthcare. There is very little scope to do anything that we’re not told to do from above — and, of course, that’s why I was sacked. Because even if you challenge — even if you just raise an intellectual question about the policy — they don’t like it.
It probably doesn’t come as a surprise to you that I’m quite a fan of Huxley. But my favourite book is not Brave New World or Doors of Perception. It’s actually Island, his last book. It is a roadmap to a society where you use psychology — you use dance, you use movement, you use exercise — and you use psychedelics to maximise quality of life. That’s what we should be doing. I was on the Good Read programme about six years ago, and Island was my Good Read. And two weeks later, I was in Parliament, at a group on drugs and drug addiction, and I was viciously attacked by a drug service provider for daring to talk on the radio about the use of illegal drugs to help people have a better life. That exemplifies our silos of thinking, which have become entrenched over decades. I don’t even think psychedelics could open their minds.
FR: When people are having these transcendent experiences on psychedelics, are they finding something that we have all lost? Barely 3% of the country goes to church anymore; we’ve lost so much of our connection to the spiritual. Do you think they are recovering some of that?
DN: Yes, I have no doubt. Psychedelics increase connectedness — with the self, with other people and with nature. There’s a very interesting relationship between psychedelics and religion, because pretty much all religions emerged from groups of people using psychedelics. Hinduism came from a combination of mushrooms and Ephedra. South American beliefs came from ayahuasca and DMT and also from mushrooms. There’s a wonderful study going on in the States using psilocybin on priests who’ve lost their faith, and it’s working — it’s working for some faiths: I don’t think it’s quite as good for Islam as it is for Christianity — but there are priests coming out saying they have begun to find their faith again.
And of course, there was this remarkable experiment called the Marsh Chapel Experiment at Harvard in the Sixties. They took trainee priests on Good Friday — when they’re going to be in chapel praying and contemplating for the whole day — and they split them and gave 10 of them psilocybin in the same doses. And of the 10 given psilocybin, eight of them have this powerful mystical experience where they saw God.
So that does help make sense of the way in which religion or religious beliefs can be facilitated by changing the way your mind works. Of course, historically, people have done that in very different ways. In the old days, you used to starve yourself for days and nights, or kneel and pray for hours and hours, to get those kinds of mystical changes. And they would have been produced by alterations in biochemistry — due to stress — which are not necessarily very different from those that psychedelics produce. But psychedelics are just easier and probably more effective.
FR: If these drugs did become widely available, how would we preserve this connection to spiritual well-being?
DN: There’s a really interesting experiment going on in the US now. Oregon has made magic mushrooms effectively a legal medicine. But more than that, they are authorising wellness centres, all around the state, to provide mushroom therapy, or mushrooms as part of wellbeing therapy. Now, that’s an amazing decision. It’s the first time anywhere in America that there’s kind of socialised medicine — using what it is now, and will be even when the therapy centres are open, an illegal drug. The purpose is to improve wellbeing in communities, and I think it’s going to work.
FR: You’re a good advocate for psychedelics, but have you faced judgement from your academic peers? Do you find that you are in any way isolated in that community?
DN: About five years ago, I gave a talk to the Royal College of Psychiatrists and about psychedelics as the future of psychiatry. And after the talk, the room divided into three separate groups. There were about seven or eight men in the room older than me, who said: “Fantastic. I was there in the Sixties, we were using it. It was working fine. Thank goodness you’re bringing it back.” And the majority of the room were people from 35 to 60 who said: “This is rubbish. There’s no RCTs. They’re dangerous drugs.” And then there were about 50 trainees who said: “Fantastic — at last. Psychiatry has got something to offer me!” So credibility is very age-related.
Academically, I’ve been generally pleasantly surprised by the positivity. I think there are a lot of academics out there who realise that this is the way forward. They just don’t have the courage to stand up and do it because they don’t want to be vilified, they don’t want the Daily Mail writing about them. But they are on-side. There’s very little criticism within the scientific community about what we’re doing, because it’s good science. It’s published in the top journals. It’s very hard to argue with that.
FR: Let’s take some questions from the audience.
You spoke about shutting down the “default mode network” as a one-off event. Have you found that there’s a need to link therapy, psychotherapy, and a deep understanding of people’s trauma with the psychedelic experience, versus treating it like a neuroscientific event?
DN: What I find amazing is that both are true and that’s why it’s unusual. In fact, it’s kind of unique in psychiatry — to be able to do a brain imaging of someone who’s had a treatment, and see why it’s worked. What we see in people who’ve been depressed, who’ve had a psychedelic trip, is their brains are more flexible. And that accords extremely well with the cognitive experience of actually being able to think differently and not be locked into negative thought loops.
But I absolutely agree with you that the experience itself is what people want to talk about — and the value of that, in terms of helping them change their lives and move forward is, for the patient, absolutely central. Critics say: “Prove to me that what the patient thinks matters.” In fact, there are people who’ve said to me: “I’m not going to believe that psychedelics work until you give it to people under anesthetic, because it could all be placebo.” It’s surreal, because we don’t do any other kind of therapy under anaesthesia. People want to talk about why the experience is valuable to them. They want to get other people to engage with it.
FR: Placebo is a concept that’s totally vilified in the mainstream scientific arena. Do you think that there’s room for a good placebo effect?
DN: Half of everything any doctor does to you is placebo. It’s you wanting to get better. If you don’t want to get better, you won’t get better. If you want to get better, you can get better, and psychedelics allow you to get better — whether that’s a placebo, or whether it’s a drug effect. I think it’s a drug effect, but proving it’s a drug effect is kind of pointless, and probably impossible, and I’m not going to bother.
I was a government minister in the Department of Health in 2018, when we rescheduled THC for therapeutic use. And probably the most important thing was having a cause célèbre. There was Billy Caldwell, and a number of children with horrendous, untreatable epilepsy — suffering dozens of fits a day — who were treated by these medicines. And the compassionate power, forced on people in positions of power, was irresistible. That is actually what led to change. So applying that to psychedelics — who will be the cause célèbre?
DN: Australia decided in February that, from the first of July, psilocybin for treatment-resistant depression, and MDMA for treatment-resistant PTSD, will be approved medicines. And that was driven by an example: a woman who was actually a friend of the Prime Minister’s husband became severely depressed, begged for psychedelic therapy, couldn’t get it, and killed himself. And she made videos and she campaigned and she became the cause célèbre because of her dead husband.
We haven’t got that patient in Britain. But the sad thing is, we do have a lot of veterans who are medicating themselves. Some of them have been part of our studies. We’ve been working with them for eight years. They have been campaigning for this law change. And it’s not happening. These veterans are going to South America to get treatment — many of them can’t afford it; we’ve got senior members of the military arguing for this. But it’s falling on deaf ears. And I don’t know what the problem is. It may be because it’s not a child. The other thing about Billy Caldwell is that he was dying in St. Thomas’s, which is just across the river from politics. Parliamentarians could not avoid the fact that he could be dead within a few hours. So they had to do something. We don’t have quite the same immediacy.
I feel that cannabis has got stuck. It’s got stuck at this stage where unlicenced cannabis medicines are massively on the rise, but the NHS is not prescribing the licenced medicine. And it’s very hard to change. Even if tomorrow, the Home Office looked to reschedule psilocybin, we’ll end up in a similar place — where psilocybin therapy is only accessible privately because the NHS won’t endorse it. What’s your view on how we push past that?
DN: You’re quite right: for four and a half years cannabis has been a medicine, and there have been four prescriptions on the NHS. That’s almost as big of a scandal as having made it illegal in the first place in 1971. The NHS is not flexible and the mistake made was to insist that cannabis could only be prescribed by a specialist. And most specialists are old white men like me who spent their lives working on treatments which aren’t cannabis, and they don’t want to have to get out of their rut and learn about cannabis. The people that need to prescribe medical cannabis are the GPs and they’re not allowed to.
The other problem with the NHS is their budgets are controlled by pharmacists.You’d think pharmacists would be interested in pharmacology, but actually they’re not — they’re interested in money, and they’re really resistant to bringing in new treatments. So even with patients where it’s incontrovertible — the consultant says: “Medical cannabis has helped this person, please can we prescribe on the NHS” — the pharmacist says: “No because NICE hasn’t approved it.” And that’s why I left the NHS. That’s why now my work with ketamine is outside the NHS. Because it’s the only way we can actually use a psychedelic drug on patients. The same will be true with psilocybin or MDMA when they become available.
What we’re doing in the clinics that I’m working with — the awakened clinics here — is collecting data. At some point in the not-too-distant future, we will be able to go to the NHS and say: “100 patients with depression treated with ketamine therapy. Make NICE approve it.” We’re all campaigning to get NICE to accept that this real-world data for ketamine could be used — in the same way that real-world data for cannabis was collected.
I work at the Centre for Social Justice and we work with around 800 small grassroots charities, many of which are working in the addiction sector. And I have yet to meet a single one of those organisations that thinks legalisation is the answer. In fact, they actually think the opposite. We recently held a roundtable with a load of drug dealers, and we asked them what they thought about legalisation, and they said they were absolutely desperate for it, because it was going to significantly increase the number of people who will be buying drugs. And their response to that, they said, would be to undercut the legal drugs by making them cheaper, and then they can make them stronger or weaker, depending on what the clients want. And I wondered what you thought of that?
DN: Free markets are a problem, aren’t they? So my argument would be that we should decriminalise personal possession of all drugs. Criminalising people who use drugs is both immoral and ineffective. It would be economically sensible to have regulated markets for all drugs which are less harmful to the user than alcohol. Because reducing the use of alcohol would have a net beneficial effect on society. We’re beginning to see that now, in countries or states where medical cannabis has become legal: people are drinking less, and also using less opiates.
In our medical cannabis initiative — the Drug Science 2021 initiative, which you can access online — we had 3,500 people on medical cannabis, over 1000 of them for chronic pain. And they almost halve their use of opiates without even being asked to stop opiate painkillers. They’re just stopping because medical cannabis is better for pain.
In terms of treatment providers, the reason cannabis is a problem in Britain is because we tried to get rid of cannabis, in the same way that heroin is a problem in America because they tried to get rid of heroin. They tried to stop people using relatively mild forms of cannabis and what did the market do? The market just shifted to make stronger forms of cannabis. When we tried to clamp down on cannabis in prisons, what happened? We started making spice, and spice kills people; cannabis doesn’t. So our hostility to cannabis has driven the problem for cannabis. When we tried to stop the use of opium in 1910 by Chinese people in the East End of London, what happened? They stopped smoking opium; they started injecting morphine.
Almost every drug we’ve tried to control through prohibition has resulted in the use of stronger, more toxic alternatives, and lead to greater problems with addiction. I was in a huge conference in Orlando, speaking to 2,500 addiction service providers, last year. I started talking about using psychedelics to treat addiction and they were horrified. But it’s their business. The addiction business is a big business. A lot of people get their employment out of it, but they need addicts to keep the business going. And if we can get rid of addicts, they will be out of business, so they don’t want change either.
When the default mode network is switched off, how does it come back? And if it comes back, how does it not cause the depression again?
DN: It comes back different, it comes back more flexible, it comes back less entrenched. Now why that is? We don’t know. One analogy is, if you keep thinking something, it’s like a cartwheel going along in a muddy field. It digs deeper and deeper and deeper. But then if you have a rainstorm or a flood, you can wash the ruts away and you can start again. But how that actually translates into neurochemical changes, or neurological changes in neurons, is still a mystery, and it is actually to my mind the big target at present. I would really like to understand how we get rid of it. Some people use the analogy of a snow field: once you’ve skied for a long time, you get stuck in a rut. Then the snow comes and you can see normally again. But eventually, for many people who’ve been chronically depressed, particularly from childhood, there’s a pressure to rut again. And what is that? I don’t know. And that’s one of the areas I’m really trying to get my head around intellectually, because then we might be able to design some experiments to test it.
FR: This comes back to this idea of neuroplasticity, which you have when you’re young and then you lose as you get older — do you think people have a fear of the general public becoming more neuroplastic?
DN: Yes and no. No one minds people with Alzheimer’s getting more neuroplastic. But young people thinking differently — that frightens society, or the establishment. But neuroplasticity — this is an ancient concept. Every time you do anything, you’ve grown a few synapses in your brain, you’ve consolidated some synapses, you’ve made them more efficient. Now, that process is very powerfully stimulated by psychedelics. It’s also stimulated by ketamine and MDMA. And from the insights you get during a trip, people often see things very differently, come up with new solutions to old problems. But they can consolidate those new solutions by neuroplasticity.
The US Department of Defence has invested something like $27 million in trying to develop drugs which will produce plasticity, without being psychedelic, because they’re terrified of psychedelics. If you’re a vet in America, and you use an illegal drug to get better, you lose your pension, and you lose your access to healthcare. So rather than change the law, they’re trying to find drugs which will actually heal the brain through plasticity. I don’t know if that’s going to work. I think it might be useful. It might augment psychotherapy. But I think it’s going to be something you take every day. I don’t think you’re going to have a single dose of a neuroplastic agent and suddenly you’re going to wake up the next morning feeling un-depressed. But the research is going on, and we’ll find out.
What is monkey dust?
DN: Monkey dust is a new cathinone. Here’s a story. Just before the 2010 election, along comes mephedrone (“meow meow” or MCAT), a relatively weak cathinone that’s legal. It becomes very popular. But an election’s coming up, and Gordon Brown doesn’t want to be seen as soft on drugs. So mephedrone gets banned. And then, after a couple of years, we start to look at the data. And what we saw with mephedrone between 2008 and 2010 was as use went up, cocaine deaths fell, amphetamine deaths fell. Why? Because people were switching from an illegal, dangerous, harmful drug, to a legal, less harmful drug. So there were two or three deaths from mephedrone, and it reduced cocaine deaths by about 50%. It’s the biggest impact on cocaine death ever.
When mephedrone is illegal, and the dose and supply runs out, people switch back to cocaine because it’s a better drug. If everything’s illegal, why not use a better drug. Cocaine deaths have now gone up and up and they’ve now reached an all-time high. So for those two years, we saw that the drug market does have a lot of rationality. People want a drug that is fun but less harmful than the ones they’re using. So having banned mephedrone people said: “Mephedrone is pretty weedy. Why don’t we make a stronger mephedrone which we can sell in smaller amounts?” That’s monkey dust. Monkey dust is to mephedrone what fentanyl is to heroin. It’s just the product of having banned mephedrone.
Are there any studies on microdosing?
DN: Yes there are and we’ve done the best one. It’s very difficult to do because the problem with microdosing is: it’s illegal. And when we set up a microdosing study at Imperial, six years ago, we wanted to give a microdose — one microgram of LSD — to people twice a week for six weeks and see what happened. And the ethics committee said yes, but every single microdose had to be given in hospital, and they had to stay in hospital for 12 hours. We’ve never done the study because we couldn’t afford to do it.
So we did a citizen science study. We basically worked out a way of getting people to randomise their own microdoses, and that study was published last year. It shows that microdosing works — if you think you’re microdosing. So if you’re taking placebo, and you think it’s a microdose, it works. That’s the best study we have so far. It’s what you want it to be, in a way. So at present, we don’t know if microdosing works, but it doesn’t seem to harm you.
With antidepressants, you don’t know what it’s doing, but you feel better after it’s built up. With psilocybin, we can see the effect on the brain scan: it’s essentially an experience that changes the person. Are there any other drugs that are like that?
DN: It’s like surgery. It’s like a cure. Are there any other drugs like that? I suppose with some anti-cancer drugs, you might get a relatively rapid cure. But not in terms of mental health. But the idea of a sudden cure is not novel in psychiatry. When I was on the Isle of Skye 30 years ago, there was a wonderful tale there about how they used to treat depression. They used to take depressed people to the blacksmith and put their head down on the anvil and the blacksmith would take out his massive hammer and bring it down right next to their head, but not hit them. And they would get better. That seems implausible, but it’s not completely implausible, because that is a massive stress.
Pavarotti suffered from depression. And he was talking about how he overcame his depression, and he was on a plane that crashed. He said: “That near-death experience lifted my depression.” And in fact quite a lot of people who have near-death experiences say not only that their depression goes, but that they feel more spiritual. Interestingly, the brain scans of people who have near-death experiences and those after psychedelics are very similar. So the final answer to your question is that it is a psychological experience, but fundamentally it’s a biological experience, changing your psyche, and that’s why it’s so powerful. Huxley was right: your brain controls your mind. If your brain gets it wrong, as it sometimes does, change your brain. Then your mind can be free.
Disclaimer
Some of the posts we share are controversial and we do not necessarily agree with them in the whole extend. Sometimes we agree with the content or part of it but we do not agree with the narration or language. Nevertheless we find them somehow interesting, valuable and/or informative or we share them, because we strongly believe in freedom of speech, free press and journalism. We strongly encourage you to have a critical approach to all the content, do your own research and analysis to build your own opinion.
We would be glad to have your feedback.
Source: UnHerd Read the original article here: https://unherd.com/