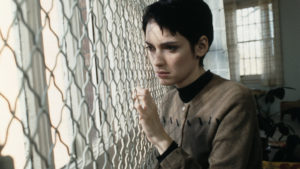
Abby walks into my office, sits down, and tells me she has been struggling with “sex addiction”. When I ask about this, she tells me of sleeping with a handful of people in the past few months at college. I try to listen supportively while also inviting her to consider her behaviour in a way that doesn’t pathologise it.
“So you think I may be delusional, or psychotic, for thinking it’s sex addiction?” She doesn’t seem to be trying to pressure me, she really wants to know. “I don’t think you’re delusional at all,” I reply. “I think you’re trying to understand yourself.”
Abby has good grades, some friends, an ex she still talks to, a few hobbies. She is nervous about her career (should she go to grad school?) and sometimes she feels sad or anxious for no reason. She is also fixated on the idea that she has a severe mental illness, possibly any severe mental illness. Having sat with her for many sessions, I am pretty sure she does not. But I also try, bearing clinical ethics in mind, to take her concerns seriously.
Abby is typical. Many young people I work with try to understand themselves (and often others) through the lens of mental illness. Typically they are focused on one diagnosis, but some, like Abby, are open to having several, many, or any. My co-workers notice it too. One colleague recently brought a question to our clinic’s staff meeting: “Has anyone else noticed a large number of students lately claiming to be on the autism spectrum, despite seeming to be… clearly not autistic based on clinical criteria?” Heads nodded. Why is it that so many young people are concerned that they are sick? And what is a mental health professional to do, in a culture where patients come in having already staked out their symptoms?
Several of my colleagues, in that meeting, suggested that teens had learned about the diagnosis they had adopted on social media. I was reminded of writer PE Moskowitz’s lamentation, last year, that mental health has become “Buzzfeed-ified”, resulting in a world where being ADHD versus being Bipolar is like being a Hufflepuff versus a Slytherin, or an Aquarius versus a Gemini. I’m not entirely convinced, though. People hear about all kinds of things on social media. To identify with what you hear requires particular conditions: you have to be searching for a convincing story to tell about yourself.
This story is about more than TikTok. The world of diagnosis is experiencing a crisis of confidence. The tools we use are somewhat reliable — we can throw the dart 20 times and hit the same spot, or 20 clinicians can meet the same person and identify that they may be “clinically depressed”. The question now is whether our tools are valid: is the bullseye actually where we think it is? If I’m debating with a college student about whether or not they have Major Depressive Disorder, I have to confront the fact that depression is not just one thing. My university students show me, over and over, that diagnoses of mental illness aren’t like medical diseases, which one either has or one doesn’t. A cluster of depressive symptoms will, in different people, have very different roots — some contextual, some biological, some behavioural. I may agree with other therapists that the patient meets the criteria for a given diagnosis, but we won’t necessarily be able to agree on what it means to have that diagnosis: where has it come from, how long will it last, what shall we do about it?
Part of the challenge lies in this very postmodern acceptance that there is no singular truth. But we do tend to end up using categories, and the ones we have currently are atavistic, more connected to the early pioneers of psychiatry than to up-to-date neuroscience. The still-common diagnosis of Borderline Personality Disorder, for instance, was constructed based on a supposed borderline between the neurotic and psychotic, which is now commonly understood as obsolete. There are myriad categories for psychotic disorders: schizophrenia, schizophreniform disorder, schizoaffective disorder, brief psychotic disorder, schizotypal personality disorder — to name just a few. Many date back to the 19th century, some are redundant, several are tough to differentiate. Some have also become politicised: during the US Civil Rights Movement, the label of schizophrenia was used to discredit black men as paranoid and violent (as Jonathan Metzl shows in his searing and meticulous history). This is just one example of how the instability of diagnostic categories stems from something far more complex than mere clinical incompetence; they are a vestige of culture and history, and they blur as times change. Psychologists and psychiatrists are so aware of this problem that it’s common, in academic spaces, to hear Plato’s phrase, “carving nature at its joints”, employed to question just how accurate our diagnostic categories are.
So why should we trust medicine to diagnose mental illness? Increasingly, we don’t. In the past, we assumed that someone would present with the question “what’s wrong with me, doctor”, and wait for a diagnosis to be handed down to them from a clinical authority. Without getting into the debate between gender critical pundits and trans liberation activists, one way in which transgender discourse has changed how we view mental health is the idea that one can self-diagnose. Part of the so-called trans tipping point is a new way of relating to medical authorities whereby patients, trans or not, come to clinics quite sure of what’s going on with them — and what they need.
This self-election is a particular sticking point in and out of the trans community. Do you have to medically transition to be trans? Do you have to have so-called “gender dysphoria” (a category recently renamed “gender incongruence”)? That these questions are even up for debate indicates a massive shift in our attitudes to diagnosis. And, critically, the centre of the debate is not in hospitals or universities but on message boards and in the writing of patients, particularly young patients, rather than clinicians.
The argument over transgender medical care often comes down to the idea that children, especially trans-identifying children, are somehow being victimised by the illegitimate or unethical authority of either pro-trans adults or gender critical adults. While some claim to be worrying about potential detransitioners, my instinct about many people’s underlying concern is the same as the one plaguing the discourse around mental health generally: who can take care of us? Who has our best interests at heart? Can we trust doctors? Does anyone really understand the boundary between sickness and wellness? The uncertainty about the answer to these questions makes almost all of us uneasy, driving us into polarised positions and moral panic.
It is tempting, especially for me as a mental health professional, to be anxious about and critical of the diminution of clinical authority. In the clinic, I frequently find myself confronted with the risks of handing the power of diagnosis to adolescents who are struggling with self-concept and inspired by two-minute confessional videos they’ve seen online. Still, when I consider the rustiness of our diagnostic categories and the ways mental healthcare, at least in the US, has been decimated by insurance companies and for-profit care, I am not sure that giving sole authority to clinicians has worked all that well either. In answering the question about who should be in charge of diagnosis, many people have good reasons for staking their positions. Many people have suffered because of inept psychiatry. But people self-diagnosing or rejecting diagnosis altogether may run into problems, too.
A paradigm shift is overdue — and appears to be beginning, though the exact shape of the future’s more democratic, more evidenced-based psychiatry is still nascent. Our ability to come up with new ideas and experiment with them will be critical. Recently the novelist Tao Lin wrote about autism spectrum disorder (ASD) that presents two radical ideas. The first is that he feels he was able to make himself “less autistic” through treatment, including recreationally using the drug MDMA. He does not describe lessening his symptoms, but rather lessening the disorder itself — flying in the face of clinical consensus that ASD is basically an unchanging brain disease.
Second, he raises serious questions about the pluralistic, inclusive, United-Colours-of-Benetton-esque view of neurodivergence, popular among the same teens filling social media with mental illness content from which my clients self-diagnose. The point is to accept and even celebrate disorders as a unique and valuable “part of you”. But Lin makes the case that there are chemical and industrial by-products that could account for the decades-long uptick in ASD, and that by uncritically embracing neurodivergence, we occlude the possibility of asking corporations and regulators to be responsible for what he believes is effectively poisoning people.
While I don’t agree with Lin word-for-word (I tend to think there are both advantages and disadvantages to pluralism, and I can’t speak to the science about the origins of autism), I did learn from his efforts to reframe these issues. His essay is a strong case for centring the voices of people who actually experience illnesses, rather than allowing the voices of clinicians to them drown out. Without listening to the people we diagnose, clinicians have time and again shown themselves to commit errors at best, and atrocities at worst.
Still, I reluctantly defend my profession’s authority. Despite there being problems within the categories we wield, our knowledge — gained both from abstract research and from simply spending careful, attentive time with hundreds and hundreds of patients — is useful in making sense of the more acutely distressing parts of what we call mental illness. The future of mental health diagnoses will have to be a negotiation between clinicians and the people they seek to treat (as well as the social and cultural context that clinicians and patients co-inhabit, which plays a critical part in how we define and experience psychological variations which then get labelled as disorders).
It won’t be easy to reach a compromise between researchers, clinicians and patients. But possible new paradigms of diagnosis are starting to emerge. There is Nonlinear Dynamical Systems Theory (NDST), for instance, which models psychiatric issues the same way we model incredibly complex ecosystems or financial markets. Within this framework, something like bipolar disorder would have multiple interlocking roots, ranging from better-understood biopsychosocial factors, such as a person’s genetic vulnerabilities, to more postmodern considerations such as the culture of a given psychiatric hospital. The relationship of these factors determines whether the mind holds steady, collapses or glitches under certain kinds of stress; understanding the interplay, in all its complexity, promotes what we might call “dynamic stability”. A skyscraper moving gently in a mild earthquake is a good metaphor for how the mind can weather certain shocks if properly prepared. While NDST is not the sole answer, it is one useful framework for pinning down, or at least functionally describing, what a diagnosis is.
A crisis of authority is not a bad thing, especially if the status quo is dysfunctional. It does, however, create anxiety. A new patient in my office last week asked me if I could capture his distress in a diagnosis. I replied that it sounded like some of his symptoms were anxious, and some were depressive, but that I didn’t have enough information to make a clear categorisation, and that the category itself might leave something to be desired.
We talked about how it felt for him to hear that. He said it was uncomfortable, but he also ventured that, without a category to make meaning for him, he would have to make meaning out of his symptoms himself. That process is what my co-workers and I are trying to enable. The aim is to help young people interpret their experiences with curiosity — even if they come to us longing for the clarity falsely promised by our flawed diagnoses.
Disclaimer
Some of the posts we share are controversial and we do not necessarily agree with them in the whole extend. Sometimes we agree with the content or part of it but we do not agree with the narration or language. Nevertheless we find them somehow interesting, valuable and/or informative or we share them, because we strongly believe in freedom of speech, free press and journalism. We strongly encourage you to have a critical approach to all the content, do your own research and analysis to build your own opinion.
We would be glad to have your feedback.
Source: UnHerd Read the original article here: https://unherd.com/